When ulcers of the lower extremity develop, it is important to find out why. Many ulcers develop over boney prominences which are subjected to pressure, and are therefore labeled as pressure ulcers. However, one common etiology of lower extremity wounds is frequently not considered, particularly in elderly persons. This is atherosclerotic disease of the lower limbs, also called peripheral arterial disease, or PAD. The term PAD can also apply to atherosclerotic disease in other locations such as carotid arteries leading to the brain. Risk factors for peripheral arterial disease include diabetes mellitus, hypertension, smoking, and hyperlipidemia.
Diagnosing PAD is important, as treatment can begin with antiplatelet therapy, vasodilators, or surgical therapies such as angioplasty and bypass grafting. Many complications related to PAD can be prevented with basic foot care, control of risk factors, timely treatment of ulceration, and interdisciplinary collaboration between nutritionists, nurses, physicians, and other specialists such as podiatrists and vascular surgeons. Persons with PAD also have increased prevalence of heart attack and stroke, making control of risk factors a major priority.
Physical signs of PAD include diminished pulses, delayed capillary return, coolness, and chronic changes of the skin such as hairlessness, pallor and thinning. When diagnosing vascular ulcers, it is important that bedside physical diagnostic signs be supplemented by objective measurements obtained by a competent vascular technician.
 Several non-invasive vascular studies are available, including transcutaneous oxygen measurement, segmental Doppler studies, skin temperature, and segmental pressures. Two of the most useful and readily available studies are ankle-brachial index and plethysmography, which translates arterial pulsation in the lower extremity into visible wave forms (pulse volume recordings or PVRs) using inflated cuffs at various levels.
Several non-invasive vascular studies are available, including transcutaneous oxygen measurement, segmental Doppler studies, skin temperature, and segmental pressures. Two of the most useful and readily available studies are ankle-brachial index and plethysmography, which translates arterial pulsation in the lower extremity into visible wave forms (pulse volume recordings or PVRs) using inflated cuffs at various levels.
Ankle-brachial index is a measure of ankle systolic pressure divided by brachial systolic pressure. A normal ratio is 0.9 to 1.3, and a ratio less than 0.9 indicates a decrease in ankle blood flow relative to the arm. An ABI less than 0.5 indicates severe occlusive disease to the leg, however this result is less reliable when arteries are stiff, as occurs when calcification is present. It is therefore advisable to use other studies to supplement ABI such as plethysmography.
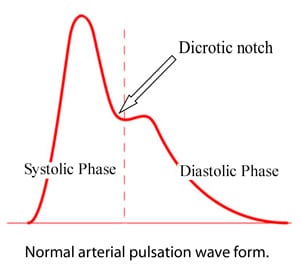
The normal pulse volume wave form shows a systolic upstroke with sharp peak, followed by a downstroke with a dicrotic notch. The figure above shows a normal pulse volume recording. Changes in contour that indicate PAD include diminution of pulse amplitude, blunted amplitude of the waveform, and absence of dicrotic notch. With severe PAD, pulsation is absent and wave forms are flattened.
Once non-invasive vascular studies are obtained which demonstrate PAD, the issue of etiology of lower extremity ulcer becomes clearer. For example, a foot ulcer in the presence of good blood flow is more likely to be a pressure ulcer, while an ulcer in the presence of severely limited blood flow can accurately be termed a vascular ulcer. When diagnosing vascular ulcers, it is important that bedside physical diagnostic signs be supplemented by objective measurements obtained by a competent vascular technician.
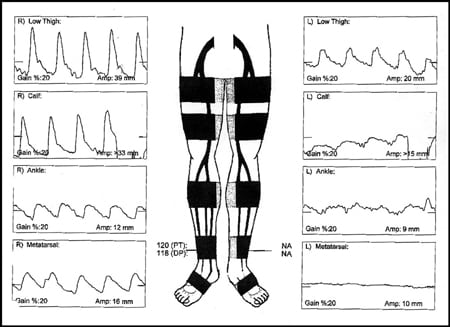
The diagram above illustrates a PVR test from an 85 year old man with history of smoking and hypertension who came to my hospital with painful ulceration to his left ankle. The right thigh appears normal but there is dampening of the wave form in the right lower leg and foot. The left leg shows abnormal wave form from the thigh down, and the left foot shows completely absent arterial pulsation. This patient barely had blood flowing to his left foot due to severe preexisting atherosclerotic disease, which contributed to ulceration and pain.
* * * * * * * * * * * * * * * * * * * * *
This post is partially based on my article: Peripheral Arterial Disease and its Consequences: Considerations for Long-term Care, Annals of Long-Term Care, Volume 17, pp 1524-7929, 2009.
